WHO recommend that COVID-19 care pathways be established at local, regional and national levels. COVID-19 care pathways are for persons with suspected or confirmed COVID-19. A person enters the COVID-19 care pathway after s/he is screened, based on a standardized case definition, including assessment of symptoms, and meets criteria for a suspect case.
Remarks:
- All persons with suspected, probable, or confirmed COVID-19 should be immediately isolated to contain virus transmission.
- Considerations for co-infections and/or chronic diseases must be made within the COVID-19 care pathway.
- All suspect cases should be tested to determine if they are a confirmed case. Until proven negative, all suspected cases should remain in the COVID-19 care pathway. If testing is not available, the person becomes a probable case (based on clinical suspicions) and should be cared for in the COVID-19 pathway.
- Discontinue transmission-based precautions (including isolation) and release from the COVID-19 care pathway as follows:
- For symptomatic patients: 10 days after symptom onset, plus at least 3 days without symptoms (without fever and respiratory symptoms).
- For asymptomatic patients: 10 days after test positive.
- Note: Known risk factors for rapid deterioration, severe disease, and/or increased mortality are older age (> 60 years) and NCDs such as cardiovascular disease, diabetes mellitus, chronic lung disease, cancer, and cerebrovascular disease (17). Patients with one or more of these risk factors should be monitored closely for deterioration
- Presenting signs and symptoms of COVID-19: Most persons experience fever (83–99%), cough (59–82%), fatigue (44–70%), anorexia (40–84%), shortness of breath (31–40%), myalgias (11–35%). Other non-specific symptoms, such as sore throat, nasal congestion, headache, diarrhoea, nausea and vomiting, loss of smell (anosmia) or loss of taste (ageusia) preceding the onset of respiratory symptoms has also been reported.
- Other complications that have been described in COVID-19 patients include acute, life-threatening conditions such as: acute pulmonary embolism, acute coronary syndrome, acute stroke and delirium. Clinical suspicion for these complications should be heightened when caring for COVID-19 patients, and appropriate diagnostic and treatment protocols available.
Dos and Don’ts according to WHO guidelines:
Instructions for patients: Ask the suspected patient to wear a medical mask and to cover nose and mouth during coughing or sneezing. Isolate the patient and keep at least 1 m distance between patients.
Apply contact and droplet precautions: For suspected and confirmed COVID-19 patients, contact and droplet or airborne precautions should be applied. Contact precautions prevent direct or indirect transmission from contact with a suspect or confirmed COVID-19 patient and/or contaminated surfaces.
Collection of samples: For all suspect cases, collection of upper respiratory tract (URT) specimens (nasopharyngeal and oropharyngeal) for testing by (RT-PCR) and, where clinical suspicion remains and URT specimens are negative, to collect specimens from the lower respiratory tract (LRT) when readily available (expectorated sputum, or endotracheal aspirate/bronchoalveolar lavage in ventilated patient). In addition, testing for other respiratory viruses and bacteria should be considered when clinically indicated.
SARS-CoV-2 antibody tests are not recommended for diagnosis of current infection with COVID-19.
Depending on local epidemiology and clinical symptoms, test for other potential etiologies (e.g. malaria, dengue fever, typhoid fever) as appropriate.
Management of covid with Mild infection: (pneumonia treatment)
Treatment: WHO recommend patients with mild COVID-19 be given symptomatic treatment such as antipyretics for fever and pain, adequate nutrition, and appropriate rehydration.
Patient counselling: Counsel patients with mild COVID-19 about signs and symptoms of complications that should prompt urgent care.
WHO recommend against antibiotic therapy or prophylaxis for patients with mild COVID-19.
Management of covid with moderate infection: (pneumonia treatment)
Isolation and hospital care: WHO recommend that patients with suspected or confirmed moderate COVID-19 (pneumonia) be isolated to contain virus transmission. Patients with moderate illness may not require emergency interventions or hospitalization; however, isolation is necessary for all suspect or confirmed cases.
Drug prescription: WHO recommend for patients with suspected or confirmed moderate COVID-19, that antibiotics should not be prescribed unless there is clinical suspicion of a bacterial infection.
Management of covid with severe infection: (pneumonia treatment)
Well-equipped facility: Areas should be equipped with pulse oximeters, functioning oxygen systems and disposable, single-use, oxygen-delivering interfaces (nasal cannula, Venturi mask, and mask with reservoir bag).
Oxygen therapy: Immediate administration of supplemental oxygen therapy to any patient with emergency signs and to any patient without emergency signs and SpO2 < 90%.
Monitor the signs and symptoms: Closely monitor patients for signs of clinical deterioration, such as rapidly progressive respiratory failure and shock and respond immediately with supportive care interventions.
Use cautious fluid management in patients with COVID-19 without tissue hypoperfusion and fluid responsiveness.
Management of critical COVID-19: septic shock
Recognize septic shock in adults when infection is suspected or confirmed AND vasopressors are needed to maintain mean arterial pressure (MAP) ≥ 65 mmHg AND lactate is ≥ 2 mmol/L, in the absence of hypovolaemia.
- In resuscitation for septic shock in adults, give 250–500 mL crystalloid fluid as rapid bolus in first 15–30 minutes.
- In resuscitation for septic shock in children, give 10–20 mL/kg crystalloid fluid as a bolus in the first 30–60 minutes.
NOTE: Fluid resuscitation may lead to volume overload, including respiratory failure, particularly with ARDS. If there is no response to fluid loading or signs of volume overload appear (e.g., jugular venous distension, crackles on lung auscultation, pulmonary oedema on imaging, or hepatomegaly), then reduce or discontinue fluid administration. This step is particularly important in patients with hypoxaemic respiratory failure.
Do not use hypotonic crystalloids, starches or gelatins for resuscitation.
In adults, administer vasopressors when shock persists during or after fluid resuscitation. The initial blood pressure target is MAP ≥ 65 mmHg in adults and improvement of markers of perfusion. (Reference)
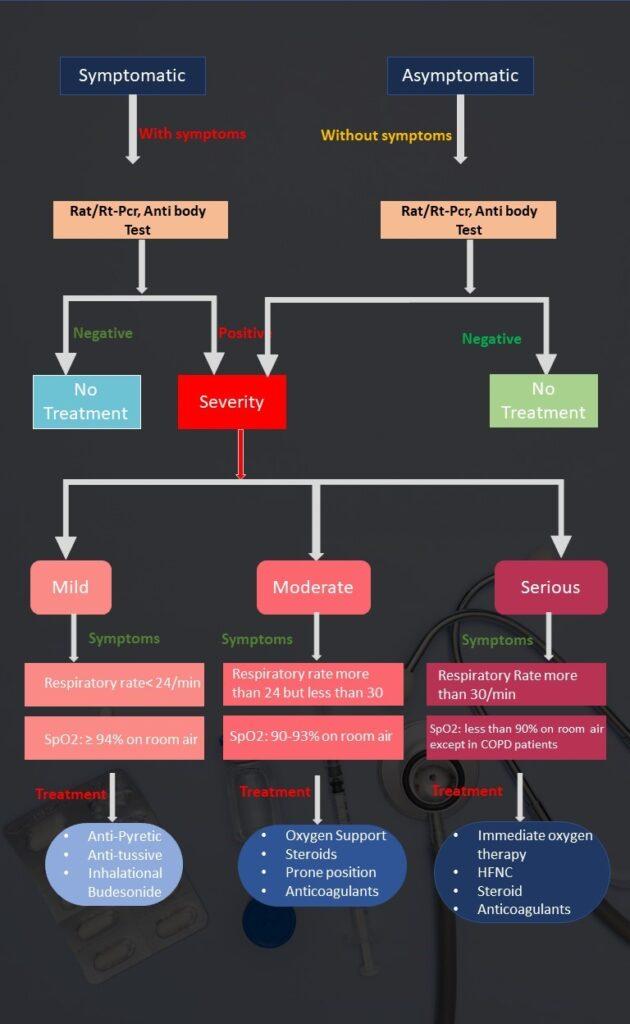
Asymptomatic Cases
- Suspected contact [RAT or RTPCR negative or not available]
- Incidentally detected [RAT or RTPCR positive]
- Take 6 min walk test as per details in 6-minute walk test at a glance
Investigations: Usually, no investigation required at this stage
Treatment
- No medication required for COVID-19 infection
- Continue medications for other co-morbid conditions if any
- Promote tele consultation by patient
- Promote COVID appropriate behaviour (mask, strict hand hygiene, physical distancing)
- Advise healthy balanced diet with proper hydration
- Advise patients and family to stay connected and engage in positive talks through phone, video-calls, etc.
Mild Cases
- No shortness of breath
- No difficulty in breathing
- Respiratory rate< 24/min
- SpO2: ≥ 94% on room air
- Take 6 min walk test as per details in 6-minute walk test at a glance box.
- For other symptoms please refer to COVID-19 symptoms at a glance box
Investigations: Patient may have to be investigated further If symptoms persist or deteriorate.
Treatment
- Promote COVID appropriate behaviour (mask, strict hand hygiene, physical distancing)
- Advise healthy balanced diet with proper hydration
- Advise patients and family to stay connected and engage in positive talks through phone, video-calls, etc.
- Self-monitoring for fever, breathlessness, SpO2 or worsening of any symptoms
- Anti-Pyretic and Anti-tussive for symptomatic relief
- Inhalational Budesonide (given via Metered dose inhaler with space device) at a dose of 800 mcg BD for 5 days) for cough
- No other COVID-19 specific medication required.
Moderate
- Shortness of breath
- Difficulty in breathing
- Respiratory rate more than 24 but less than 30
- SpO2: 90-93% on room air
Treatment
- Oxygen support to be titrated to maintain SpO2 between 92%-95% in patients without COPD
- Initial device for oxygen administration (nasal prongs, simple face mask or NRB mask) depends upon severity of hypoxia and work of breathing.
- In case of COPD, oxygen therapy may not be required as target SpO2 is between 88%-92% which by definitions of moderate cases is already present.
- Control of co-morbid condition especially diabetes.
- Steroids must be given if SpO2 is below 92%. See details in Drug Therapy Guide Box
- Proning helps in better oxygenation of lungs
- Further treatment by steroids, anticoagulants and/or of immune modulators shall be guided by the results of the baseline and repeat investigations.
- Prophylactic doses of anti-coagulants such as LMWH or unfractionated heparin.
Severe Cases
- Shortness of breath
- Difficulty in breathing
- Respiratory Rate more than 30/min
- SpO2: less than 90% on room air except in COPD patients
Treatment
- Immediate oxygen therapy, initiate at 5 L/Min and titration to reach target SpO2 ≥ 90% in nonpregnant adults and 92-96% in pregnant patients.
- Consider use of NIV (Helmet or face mask interface depending on availability) in patients with increasing oxygen requirement.
- Consider use of HFNC if patient does not improve.
- Consider intubation& mechanical ventilation if patient still does not improve or work of breathing is extremely high.
- Start steroid therapy.
- Obtain baseline investigations and repeat the same as per investigation box below.
- Further treatment by steroids, anti-coagulants and/or of immune modulators shall be guided by the results of the baseline and repeat investigations.
- Prophylactic doses of anticoagulants such as LMWH or UFH eg 40 mg enoxaparin S/C daily. Anticoagulants may also be administered based on clinical judgement.
Guidelines for use of Remdesivir
Remdesivir is used only in select moderate/ severe hospitalised COVID-19 patients on supplemental oxygen within 10 days of onset of disease. It should not be used in mild cases and must be prescribed by senior faculty member with great caution.
Guidelines for use of Tocilizumab
It is an immunosuppressant drug ONLY in severe and critically ill patients of COVID-19. If no signs of improvement is shown in terms of oxygen requirement even after 24-48 hours of administration of steroids.
Patient should be free of any bacterial/ fungal/ tuberculous infection at the time of administration of Tocilizumab.
Guidelines for use of Steroids
It should only be given to hospitalized moderately severe and critically ill COVID-19 cases.
Monitoring of blood glucose is mandatory in all patients put on steroids as it may precipitate hyperglycaemia.
Self-medication of steroids must be avoided.
Guidelines for use of Anti-coagulants
Moderate cases: Prophylactic doses to be used with un-fractionated heparin or low molecular weight heparin (weight based e.g., Enoxaparin 0.5 mg/kg per day SC OD).
Moderate cases: Prophylactic doses to be used with un-fractionated heparin or low molecular weight heparin (weight based e.g., Enoxaparin 0.5 mg/kg per day SC OD), therapeutic dose to be used only if there is evidence of thromboembolism.
Rational use of HRCT imaging guide box
It provides better visualization of the extent and nature of lung involvement in patients with COVID-19.
Suspected and confirmed cases of moderate COVID-19 who continue to deteriorate clinically even after initiation of appropriate therapy especially when there is high risk of invasive fungal infection.
Treating Physician/ Intensivist may consider HRCT chest depending on clinical assessment of the patient.
Situations when HRCT imaging of Chest should not be done: For diagnosing/ screening Covid-19 infection, it is also not required to initiate treatment in COVID-19 patients with hypoxia and an abnormal chest radiograph, not in assessing the response to treatment.
Managing Mucormycosis
According to the recent research there is a significant increase in the number of cases of Mucormycosis in Covid – 19 patients during treatment in hospitals and after discharge in different parts of the country. It is a complication caused by fungal infection.
Time of presentation: variable but usually around 3rd week of onset of symptoms of Covid – 19.
Reasons for increase in Mucormycosis in Covid – 19 patients: Hyperglycemia, irrational or overuse of steroids in management of covid, irrational use of broad-spectrum antibiotics, Pre-existing co-morbidities such as haematological malignancies, use of immunosuppressants, solid organ transplant.
Signs and symptoms:
- Facial pain, pain over sinuses, pain in teeth and gums
- Paraesthesia / decreased sensation over half of face.
- Blackish discolouration of skin over nasolabial groove/ alae nasii.
- Nasal crusting and nasal discharge which could be blackish, or blood tinged.
- Conjunctival injection or chemosis.
- Periorbital swelling.
- Blurring of vision/ diplopia.
- Loosening of teeth/ discoloration of palate/ gangrenous inferior turbinates.
- Worsening of respiratory symptoms, haemoptysis, chest pain, alteration of consciousness, headache.
Investigation:
- KOH mount and microscopy, histopathology of debrided tissue (presence of Ribbon like aseptate hyphae 5-15 µ thick that branch at right angles)
- NCCT PNS (to see bony erosion)
- HRCT chest (≥ 10 nodules, reverse halo sign, CT bronchus sign etc.) and CT Angiography
- MRI brain for better delineation of CNS involvement
Management:
- Timely initiation of treatment reduces mortality. Treatment involves combination of surgical debridement and antifungal therapy.
- Liposomal Amphotericin B in initial dose of 5mg/kg body weight (10 mg/kg body weight in case of CNS involvement. It should be diluted in 5%dextrose.
- Conventional Amphotericin B (deoxy cholate) in the dose 1-1.5mg/kg may be used if liposomal form is not available.
- Kidney Functions must be monitored during the entire management period. (Reference 2)