(BELOW 18 YEARS)
Severity of condition
- Asymptomatic: It is assumed that third wave might infect the children more than any other age group. The part to be concerned about is that most cases reported are asymptomatic.
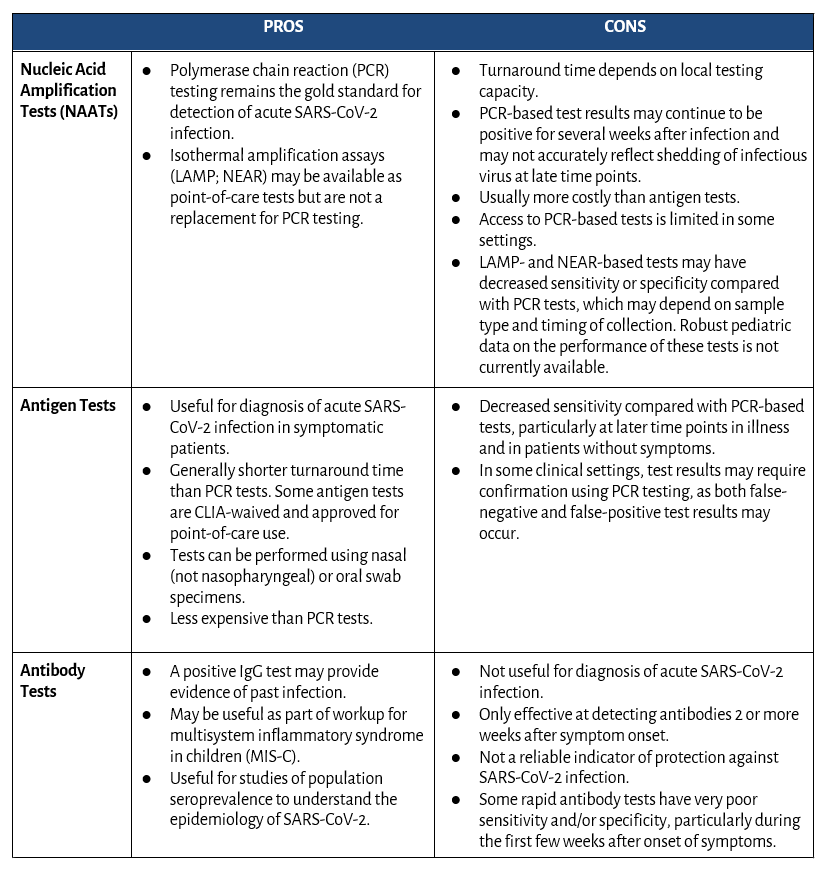
- Diagnosis: Antibody test, RAT or RTPCR, 6 minutes walk test in children above 12 years of age
- Treatment: No specific medicine for covid-19 infection, Continue medications for other condition if any
- Precautions: Promote COVID appropriate behavior like; strict hand hygiene, physical distancing.
- Create positivity around patient by communicating and engaging in the activities.
- Give them proper rest or sleep for not less than 8 hours
- Mild Cases:
Symptoms:
- Sore throat or rhinorrhea
- Cough with no breathing difficulty
- SPO2 ≥ 94% on room air
Diagnosis: Take 6 min walk test in children above 12 years under
supervision of parents/guardian
Treatment:
- For fever- Paracetamol 10-15mg/kg/dose
- For cough: Throat soothing agents and warm saline
- gargles in older children and adolescents
- Fluids and feeds: Ensure plenty of oral fluids to maintain hydration along with nutritious diet
- No other COVID-19 specific medication needed
- Antimicrobials are not indicated
Precautions: Regular monitoring of respiratory rate 2-3 times a day, look for chest indrawing, bluish discoloration of body, cold extremities, urine output, oxygen saturation, fluid intake, activity level, especially for young children
3. Moderate Cases: In addition to symptoms in mild cases, check for
pneumonia which may not be apparent
- Rapid respiration (age-based): <2 months RR >60/min;
- 2-12 months, RR >50/min; 1-5 years, RR >40/min;
- >5 years, RR >30/min
- SpO2: 90-93 % on room air
Treatment:
- Initiate immediate oxygen therapy
- Maintain fluid and electrolyte balance
- Encourage oral fluids (breast feeds in infants)
- Initiate intravenous fluid therapy if oral intake is poor
- Anticoagulants may also be indicated
- For fever (temperature >38°C or 100.4°F): Paracetamol 10-15mg/kg/dose
- Anti-microbials to be administered if there is evidence/strong suspicion of superadded bacterial infection
4. Severe cases:
Symptoms:
- SpO2 < 90% on room air
- Signs of severe pneumonia
- Acute respiratory distress syndrome
- Septic shock or multi-organ dysfunction syndrome
- Pneumonia with cyanosis, grunting, severe retraction of chest, lethargy, somnolence, seizure
- Assess for thrombosis, hemophagocytic lymphohistiocytosis (HLH) cells of the immune system called T and NK cells do not work properly. These cells become overactive, causing too much inflammation. Ordinarily, these cells destroy infected, damaged cells of the body.
Mainstay of Treatment
- Initiate immediate oxygen therapy
- Maintain fluid and electrolyte balance
- Corticosteroids therapy to be initiated
- Anticoagulants may also be indicated
- Exercise caution and see use of corticosteroids and anti-coagulants guide
- Anti-microbials to be administered if there is evidence/strong suspicion of superadded bacterial infection.
- May need organ support in case of organ dysfunction, e.g. renal replacement therapy
Monitoring the Spo2 rate
During sleep keep the hand on child’s stomach and count the breathing
It varies with the age group:
- Upto 6 months: 30 to 60 breath per minute
- 6 to 12 months: 24 to 30 breath per minute
- 1 to 5 years: 20 to 30 breath per minute
- 6 to 12 years: 12 to 20 breath per minute
- 12 years and above: 12 to 20 breath per minute
Essential diet for children fighting with the infection
- Vegetables prepared in many ways, including steamed, roasted, in a salad or dipped in dressing or hummus
- Fresh fruits that are also rich in fiber and antioxidants
- Dairy products such as cheese or Greek yogurt
- Eggs prepared any way the child prefers
- Lean meats including poultry and fish
- Beans, nuts and seeds
- Whole wheat crackers with low-fat cheese
- Encourage children towards complex carbs such as vegetables and whole grains. Vitamins and minerals present in them will keep children healthy also helps control blood sugar levels.
Investigations in moderate and severe cases:
- Baseline lab investigations: CBC, Blood Glucose, urine routine, LFT, KFT, CRP, S. Ferritin, D-Dimer, LDH, CPK.
- Repeat investigations: CRP and D-Dimer 48 to 72 hourly; CBC, KFT, LFT 24 to 48 hourly; IL-6 (subject to availability)
- Investigations may have to be repeated more frequently in ICU settings; serial CXR should be at least 48 hours apart
- HRCT chest to be done ONLY if there is worsening of symptoms, please see rational use of HRCT imaging guide
Nucleic acid amplification test (NAAT)
- Polymerase chain reaction (PCR) tests which are highly accurate. A PCR test authorized or approved by the U.S. Food and Drug Administration (FDA) is considered the “gold standard” to determine if a child has an active COVID-19 infection.
- Loop-mediated isothermal amplification (LAMP) and nicking enzyme amplification reaction (NEAR) tests. Some of these newer tests have received FDA emergency-use authorization. Until more information is available on how well they work for children, PCR tests are not a replacement for PCR testing.
The most common scenarios in which to consider testing include:
- Patients with symptoms consistent with COVID-19
- Patients who were in close contact with a person with confirmed or probable SARS-CoV-2 infection
- Patients who require screening based on recommendations from public health authorities or other situations (eg, prior to a medical procedure such as elective surgery or as a school or workplace requirement).
Specific therapy for children
There is No role of Hydroxychloroquine, Favipiravir, Ivermectin, lopinavir/ritonavir, Remdesivir, Umifenovir, Immunomodulators including Tocilizumab, Interferon B 1 a, Convalescent plasma infusion or dexamethasone.
The COVID-19 Treatment Guidelines Panel (the Panel) recommends using dexamethasone for hospitalized children with COVID-19 who require high-flow oxygen, noninvasive ventilation, invasive mechanical ventilation, or extracorporeal membrane oxygenation.
Bamlanivimab plus etesevimab or casirivimab plus imdevimab may be considered on a case-by-case basis for non-hospitalized children who meet Emergency Use Authorization (EUA)
The Panel recommends against the use of convalescent plasma for pediatric patients with COVID-19 who are mechanically ventilated.
The Panel recommends against the use of sarilumab for hospitalized children with COVID-19 or MIS-C, except in a clinical trial.
https://www.covid19treatmentguidelines.nih.gov/special-populations/children/
Multisystem inflammatory syndrome in children (MIS-C) clinical features, evaluation, and diagnosis
Multi System Inflammatory Syndrome in Children (MIS-C) is a new syndrome in children characterized by unremitting fever >38°C and epidemiological linkage with SARS-CoV-2.
It usually occurs after 2–4 weeks of recovery from acute COVID-19 Diagnostic criteria (WHO)
Children and adolescents 0–18 years of age with fever ≥3 days
And any two of the following: Rash or bilateral non-purulent conjunctivitis or muco-cutaneous inflammation signs (oral, hands or feet)
Hypotension or shock
Features of myocardial dysfunction- pericarditis (the membrane around the heart become red and swollen), valvulitis (inflammation of valves of heart), or coronary abnormalities
Acute gastrointestinal problems (diarrhea, vomiting, or abdominal pain)
Elevated markers of inflammation such as ESR, C-reactive protein, or procalcitonin
Treatment– The child needs appropriate supportive care preferably in ICU for treatment of cardiac dysfunction, shock, coronary involvement, multi-organ dysfunction.
Drugs to be used are:
- Intravenous immunoglobulin (IVIG): 2g/kg over 12 to 24 hours
- Steroids: Methylprednisolone 1-2mg/kg/day
- High dose corticosteroid (methylprednisolone 10-30 mg/kg/day for 3-5 days); must be tapered over 2 to 3 weeks while monitoring inflammatory markers
- Aspirin: 3mg/kg/day to 5 mg/kg/day, max 81mg/day (if thrombosis or coronary aneurysm score is >2.5)
- Low molecular weight heparin (Enoxaparin): 1mg/kg twice daily
- Use of biologicals only after expert consultation and should be used at tertiary care only
For children with cardiac involvement, repeat ECG 48 hourly & repeat ECHO at 7–14days and between 4 to 6 weeks (and after 1 year if initial ECHO was abnormal)
Guidelines for wearing a mask
- Children aged 5 years and under should not be required to wear masks
- Children aged 6-11 years may wear a mask depending on the ability of child to use a mask safely and appropriately under direct supervision of parents/guardians
- Children aged 12 years and over should wear a mask under the same conditions as adults
- Ensure hands are kept clean with soap and water, or an alcohol based hand rub, while handling masks
Home care and precautions (guidelines for family)
- Wear a mask if they must be around other people. Masks should not be worn by kids younger than 5 years old or anyone who has trouble breathing.
- During cough and sneeze always cover your mouth with the tissue and throw the tissue right away into the dustbin. Wash your hands with soap and water for at least 20 seconds or use alcohol-based hand sanitizer.
- If possible, stay in a bedroom and use a bathroom separate from other people in the home.
- Use separate dishes, glasses, cups, and eating utensils and not share these with other household members. After use, run them through the dishwasher or wash with extremely hot soapy water.
- Use separate bedding and towels and not share these with other household members.
Also:
- If the person who is sick cannot wear a mask, caregivers should wear one while they’re in the same room.
- Make sure shared spaces in the home have good air flow. You can open a window or turn on an air filter or air conditioner.
- Do not allow visitors into your home. This includes children and adults.
- All household members should wash their hands well and often. Wash with soap and water for at least 20 seconds or use alcohol-based hand sanitizer.
- Wash the sick person’s clothing, bedding, and towels with detergent on the hottest temperature possible. Wear gloves when handling their laundry, if possible. Wash your hands well after handling the laundry (even if you wore gloves).
- Every day, use a household cleaner or wipe to clean things that get touched a lot. These include doorknobs, light switches, toys, remote controls, sink handles, counters, and phones. Keep a sick child’s toys separate from other toys, if possible.
- The person who is sick should stay home unless they need medical care. This is called isolation.
- Other household members also should stay home. This is called quarantine.